Table of Contents
- Introduction: Why Pain Is a Constant Companion of Cancer
- Understanding Pain: Emotional and Sensory Dimensions
- Types of Cancer-Related Pain
- Acute vs. Chronic Pain in Oncology
- The Broad Impact of Pain on Quality of Life
- Modern Approaches to Pain Management
- Vidatox: A Potential Adjunct Therapy
- Key Takeaways and Final Thoughts
- Disclaimer
1. Introduction: Why Pain Is a Constant Companion of Cancer
Cancer is a multifaceted disease that can affect almost any organ or tissue in the human body. From early detection through advanced stages, many patients experience persistent pain that can vary in intensity and duration.
While pain in other illnesses or injuries often diminishes once the underlying cause is treated, cancer pain may persist because of ongoing tumor growth, invasive treatment procedures, or chronic inflammation.
This prolonged discomfort doesn’t just stem from damaged tissue. It can also be an outcome of the body’s own defensive responses, psychological stress, and the side effects of strong medications.
As oncology continues to advance, researchers and medical professionals strive to address both the root cause of the disease and the side effects that hinder a patient’s daily life. Comprehensive pain management is a key factor in maintaining a patient’s ability to function, cope with treatments, and sustain a hopeful outlook.
2. Understanding Pain: Emotional and Sensory Dimensions
Pain is far more than just a physical sensation. It encompasses both sensory and emotional components, meaning it has a clear physiological basis but also a deeply personal, psychological aspect.
In essence, pain is the body’s built-in alarm system, signaling that something may be causing harm or damage. When pain persists over time, it can become intertwined with fear, anxiety, and depression, which can intensify the overall perception of discomfort.

In cancer, pain might emerge from the tumors themselves, from postoperative scarring, or from treatments such as radiation and chemotherapy. Beyond the physical triggers, the stress of a cancer diagnosis can amplify how patients experience pain.
Understanding these intertwined dimensions allows healthcare teams to adopt a holistic perspective. Instead of focusing solely on physical causes, many pain management strategies now integrate emotional support, mindfulness techniques, and therapy to help patients manage their symptoms on multiple levels.
3. Types of Cancer-Related Pain
Although patients might simply describe their distress as “pain,” there are different categories that clarify why it occurs and how best to relieve it. In oncology, the two primary types are nociceptive pain and neuropathic pain.
Nociceptive Pain
Nociceptive pain is triggered by the activation of specialized pain receptors, known as nociceptors, in the peripheral nervous system.
When tumors invade or press on bodily structures—such as bones, organs, or connective tissues—these receptors send alarm signals to the brain.
Nociceptive pain often feels achy, throbbing, or sharp, and can be acute or chronic depending on how long the tissue remains irritated or damaged.
Common scenarios in cancer include:
- Tumors exerting pressure on bones or soft tissues
- Postsurgical inflammation following tumor removal
- Radiation-induced irritation or burns
By identifying the role of nociceptors, healthcare providers can determine the most effective interventions, which may range from anti-inflammatory drugs to opioids, depending on severity.
Neuropathic Pain
Neuropathic pain arises from damage or dysfunction in the nervous system itself. This can include injuries to the peripheral nerves outside the spinal cord or to the central nervous system within the spinal cord and brain.
In cancer patients, neuropathic pain can develop if a tumor compresses or invades nerve pathways, or if treatments such as chemotherapy harm nerve function.
This type of pain is frequently described as burning, electrical, shooting, or tingling. It may also be accompanied by numbness or heightened sensitivity in certain areas.
Addressing neuropathic pain often requires a different approach than nociceptive pain. Medications such as anticonvulsants, antidepressants, or specific nerve-targeting treatments can help alleviate these symptoms.
4. Acute vs. Chronic Pain in Oncology

Cancer-related pain does not always present in the same way. It may be categorized as acute or chronic:
- Acute Pain: Often arises immediately after surgery or radiological procedures. Although it can be intense, acute pain typically subsides as tissues heal. It responds well to short-term use of painkillers such as NSAIDs or short-acting opioids.
- Chronic Pain: Persists for longer periods—weeks, months, or even years—and frequently stems from ongoing tumor growth, metastasis, or irreversible treatment-related nerve damage. Chronic pain can become more complex to manage as it weaves into a patient’s emotional and psychological state, sometimes requiring multi-modal therapies that combine medications, counseling, and physical rehabilitation.
The transition from acute to chronic pain can occur if interventions are not administered promptly or if the cancer itself evolves and spreads.
For this reason, specialists emphasize early assessment, frequent re-evaluation, and prompt adjustment of pain control measures.
5. The Broad Impact of Pain on Quality of Life
Cancer pain goes well beyond physical discomfort. Persistent, poorly managed pain can disrupt virtually every aspect of day-to-day life:
- Mobility and Independence: Patients may feel limited in movement, shun physical activities, and lose muscle strength over time.
- Appetite and Nutrition: Pain can diminish the desire to eat, leading to weight loss, weakened immunity, and slower recovery.
- Sleep: Ongoing discomfort can sabotage restful sleep, creating a vicious cycle of fatigue, emotional distress, and intensified pain perception.
- Mental and Emotional Well-Being: Chronic pain can contribute to anxiety, depression, and social withdrawal, causing emotional strain for both patients and their families.
Addressing these facets requires an integrated plan that involves medical treatments, counseling, rehabilitation, and social support.
When pain management is successful, patients are more likely to maintain an active lifestyle, adhere to treatment schedules, and sustain a positive mindset.
6. Modern Approaches to Pain Management
Medication-Based Therapies
A variety of pharmaceuticals can help manage or even fully control cancer pain in many cases. Clinicians often follow a “ladder” approach, starting with non-opioid drugs such as acetaminophen or NSAIDs. If these prove inadequate, they may introduce mild to strong opioids like codeine, morphine, or fentanyl.
Additionally, certain medications—such as anticonvulsants (for neuropathic pain) or steroids (for inflammation)—may be used to target specific aspects of discomfort.
Key elements of medication-based strategies include:
- Regular assessment and dose adjustments to match the patient’s changing condition
- Monitoring and managing side effects such as constipation, drowsiness, or nausea
- Educating patients and caregivers about proper usage, potential risks, and signs of tolerance or dependence
Supportive Therapies and Lifestyle Changes
Medications form the core of cancer pain treatment, but supportive approaches can substantially enhance outcomes:
- Physical Therapy: Targeted exercises, gentle stretching, and mobility training help improve blood circulation, minimize stiffness, and maintain muscle health.
- Psychological Support: Counseling, cognitive-behavioral therapy, and support groups can reduce stress, anxiety, and any sense of isolation. Mental health support often helps patients cope better with pain.
- Complementary Approaches: Methods such as acupuncture, massage, and mindfulness-based stress reduction are frequently used alongside conventional treatments. While research findings differ in their conclusions, many patients report improved comfort and relaxation.
By combining medical and holistic strategies, healthcare teams can address the diverse causes and effects of cancer pain in a more personalized manner.
7. Vidatox: A Potential Adjunct Therapy
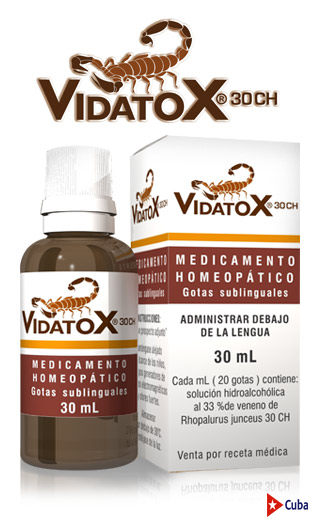
What Is Vidatox
Vidatox is a bioactive supplement formulated from the venom of the blue scorpion, an arachnid unique to Cuba. The venom is collected through specialized processes on scorpion farms, ensuring the creatures are not harmed. According to its proponents, Vidatox may help ease pain and enhance immune function in patients undergoing cancer treatment.
Potential Benefits
- Pain Relief: Preliminary studies suggest that certain peptides in blue scorpion venom may help reduce inflammation and interrupt pain signals.
- Immune Support: Vidatox proponents claim it can boost the immune system, helping the body cope more effectively with both cancer cells and the rigors of treatments like chemotherapy.
- Detoxification Aid: Some believe it assists in eliminating toxic byproducts of treatment, although comprehensive clinical evidence is still being gathered.
It is important to emphasize that Vidatox is not a recognized cure for cancer. Instead, many people view it as a complementary supplement that may offer additional relief.
Before introducing Vidatox or any new supplement into a cancer treatment plan, patients should consult with their oncologist or healthcare team to discuss potential benefits, risks, and interactions with standard therapies.
8. Key Takeaways and Final Thoughts
- Cancer Pain Is Multifaceted: It can stem from direct tissue damage, nerve involvement, or the side effects of treatments, and it affects both body and mind.
- Individualized Assessment: Identifying whether pain is nociceptive or neuropathic is crucial, as each type requires a specific therapeutic approach.
- Early Intervention Matters: Timely pain control can prevent acute pain from becoming chronic and can improve overall treatment compliance.
- Comprehensive Management: Combining medication, physical therapies, and psychological support often yields the best results.
- Vidatox as an Adjunct: Derived from blue scorpion venom, Vidatox may offer additional relief and immune support but should be used as part of a medically supervised plan.
By focusing on each patient’s unique experience and staying open to various treatment modalities, healthcare providers can help individuals facing cancer navigate pain more effectively.
This not only supports a better quality of life but can also improve treatment outcomes and emotional well-being.
9. Disclaimer
This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare professional for an individualized pain management strategy. The efficacy of supplements like Vidatox can vary greatly, and they should be discussed in detail with medical professionals to ensure they fit safely and effectively into a broader cancer treatment plan.